New Ulcerative Colitis treatments 2024
New Ulcerative Colitis Treatments 2024
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) characterized by inflammation and ulceration of the innermost lining of the colon and rectum. This condition presents with symptoms such as persistent diarrhea, abdominal pain, rectal bleeding, and an urgent need to defecate. The exact cause of UC is not fully understood, but it is thought to result from an abnormal immune response to the bacteria in the digestive tract in genetically predisposed individuals. Risk factors include family history, certain medications, and environmental factors, although none of these are definitive causes. UC is a relapsing-remitting disease, meaning that patients experience periods of active symptoms (flares) followed by times of remission when symptoms are absent.
Treatment options for ulcerative colitis aim to reduce inflammation, control symptoms, and induce and maintain remission. Medications used in the treatment of UC include aminosalicylates, corticosteroids, immunomodulators, and biologic therapies, which target specific components of the immune system. The choice of medication depends on the severity and extent of the disease, as well as the patient's response to previous treatments. Some patients may also require surgery if they do not respond to medications or develop complications. It is important for individuals to work closely with their healthcare provider to determine the most appropriate treatment plan based on their specific condition and overall health.

Treatment options
| Treatment option | Estimated cost | Efficacy | Eligibility |
|---|---|---|---|
| Aminosalicylates (e.g., mesalamine) | $300 - $600 | Effective for mild to moderate cases | Most patients with mild to moderate ulcerative colitis |
| Corticosteroids (e.g., prednisone) | $40 - $200 | Effective for moderate to severe cases | Patients with moderate to severe ulcerative colitis or those not responding to other treatments |
| Immunomodulators (e.g., azathioprine) | $200 - $500 | Can be effective for maintaining remission | Patients who do not respond to aminosalicylates or corticosteroids |
| Biologics (e.g., infliximab) | $2,500 - $5,000 | Effective for moderate to severe cases | Patients with moderate to severe ulcerative colitis, particularly those who have not responded to conventional therapy |
| Zeposia (ozanimod) | $2,500 - $3,000 | Effective for moderate to severe cases | Adult patients with moderate to severe active ulcerative colitis |
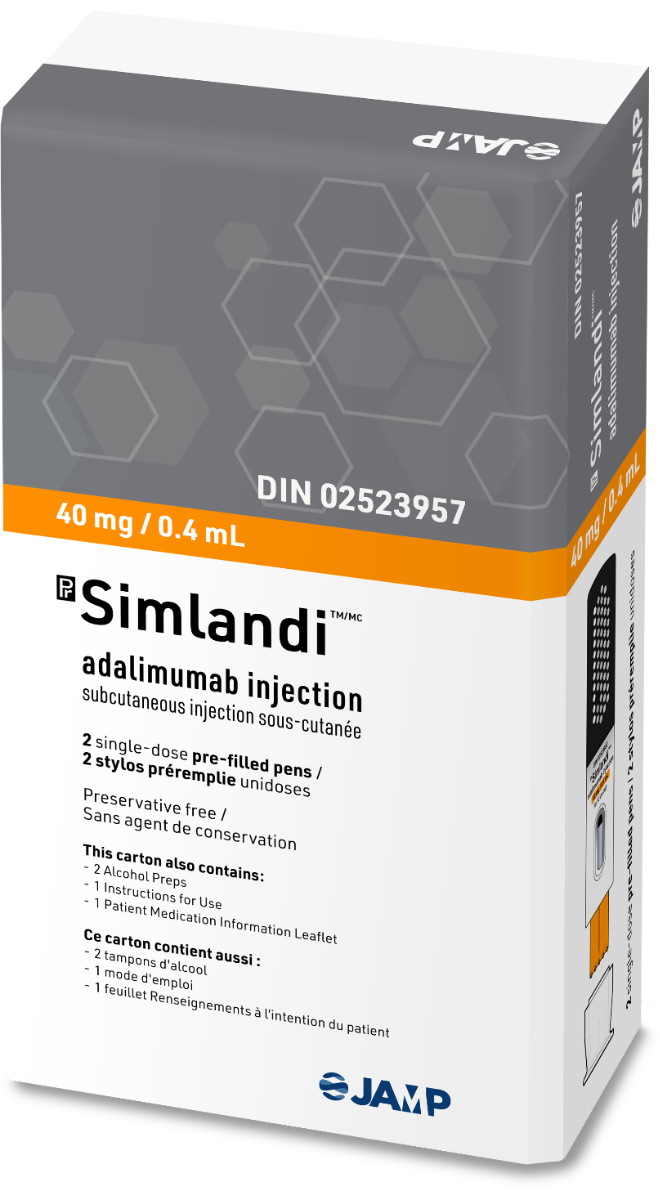
| Simlandi (not an approved drug) | Not available | Unknown | Not applicable as it is not an approved drug |
| Fecal Microbiota Transplantation (experimental) | $500 - $1,000 | Variable efficacy, more research needed | Patients participating in clinical trials |
| Surgery (e.g., colectomy) | $20,000 - $60,000 | Effective for removing diseased portion of the colon | Patients with severe ulcerative colitis or those at high risk for colon cancer |
| Dietary Changes (e.g., Specific Carbohydrate Diet) | Varies with diet | May help some patients manage symptoms | Patients looking for adjunctive treatment options |
| Stem Cell Therapy (experimental) | $10,000 - $25,000 | Still under investigation | Patients participating in clinical trials |
Treatments options in detail
Medications for Ulcerative Colitis
The treatment of Ulcerative Colitis (UC) primarily aims to reduce inflammation that causes symptoms, such as diarrhea, rectal bleeding, and abdominal pain. The most common treatments for UC include aminosalicylates, corticosteroids, immunomodulators, and biologic therapies.
Aminosalicylates
Aminosalicylates are often the first line of treatment for mild to moderate UC. These medications include drugs like sulfasalazine, mesalamine, balsalazide, and olsalazine. They work by reducing inflammation in the lining of the colon and are available in various forms, such as tablets, suppositories, enemas, and oral granules.
Corticosteroids
Corticosteroids, such as prednisone and budesonide, are used for moderate to severe UC flare-ups. They are potent anti-inflammatory agents but are not intended for long-term use due to their significant side effects, which can include osteoporosis, hypertension, diabetes, and increased susceptibility to infections.
Immunomodulators
Immunomodulators like azathioprine, 6-mercaptopurine, and cyclosporine are used for patients who do not respond to aminosalicylates or corticosteroids. These drugs suppress the immune system to reduce inflammation. They are slower to act than corticosteroids and may take several months to become effective.
Biologic Therapies
Biologic therapies are used for patients with moderate to severe UC who do not respond to conventional treatments. These drugs target specific pathways in the immune system to reduce inflammation. Biologics used in UC include tumor necrosis factor (TNF) inhibitors like infliximab, adalimumab, and golimumab, integrin receptor antagonists like vedolizumab, and interleukin-12 and interleukin-23 antagonist like ustekinumab.
Janus Kinase (JAK) Inhibitors
Tofacitinib is a JAK inhibitor approved for the treatment of moderate to severe UC. It works by blocking the signaling pathway of several enzymes involved in the immune response, thereby reducing inflammation.
Sphingosine 1-Phosphate Receptor Modulators
Zeposia (ozanimod) is a sphingosine 1-phosphate receptor modulator that has been approved by the FDA for the treatment of moderate to severe UC. It works by trapping certain white blood cells in the lymph nodes, preventing them from reaching the colon and causing inflammation.
Antibiotics
Antibiotics may be used if an infection is suspected or if there are severe flare-ups that might be related to bacterial overgrowth. However, they are not typically used as a long-term treatment for UC.
Antidiarrheal Medications and Pain Relievers
For symptomatic relief, antidiarrheal medications and pain relievers may be prescribed. However, they should be used cautiously as they can worsen certain conditions associated with UC.
Iron Supplements and Vitamins
Iron supplements may be necessary for patients with chronic intestinal bleeding who may have anemia. Vitamin B12 and other vitamin supplements might also be recommended if the patient has malabsorption issues.
Experimental Treatments
Experimental treatments for UC include stem cell therapy, fecal microbiota transplantation, and new biologic drugs that target different aspects of the immune system. These treatments are still under investigation in clinical trials and are not widely available.
Treatments Not Approved by the FDA
There are treatments available in other countries or under investigation that have not been approved by the FDA for UC. These include certain probiotics, herbal remedies, and dietary supplements. Patients should consult their healthcare provider before using any non-approved treatments.
Off-Label Use of Medications in Ulcerative Colitis
Occasionally, medications approved for other conditions are used off-label for UC. These include certain antibiotics, probiotics, and other immunosuppressive agents. The evidence for the effectiveness of these treatments varies, and they should only be used under the guidance of a healthcare professional.
Simlandi
Simlandi is not a recognized medication for the treatment of Ulcerative Colitis. It is possible that the name is misspelled or it may be a brand name not known in the context of UC treatment. Patients should ensure they have the correct information and consult their healthcare provider for advice on any medication.
Surgical Options
When medications do not sufficiently control UC symptoms, or if there are complications like severe bleeding, perforation of the colon, or cancer, surgery may be necessary. The most common surgical procedure is a proctocolectomy with ileal pouch-anal anastomosis (IPAA), which involves the removal of the colon and rectum and the creation of a pouch from the end of the small intestine to restore bowel function.
Lifestyle and Dietary Changes
In addition to medication, lifestyle and dietary changes can help manage UC symptoms. These may include eating a well-balanced diet, avoiding foods that trigger symptoms, managing stress, and quitting smoking. Each patient's triggers may be different, so individualized dietary advice from a healthcare provider or nutritionist is beneficial.
Conclusion
The treatment of Ulcerative Colitis is highly individualized and often requires a combination of medications and lifestyle adjustments. The most common treatments aim to reduce inflammation and manage symptoms, but in some cases, surgery may be necessary. Experimental treatments and off-label medication use are options under investigation or for cases where standard therapies are ineffective. Patients should work closely with their healthcare providers to determine the best treatment plan for their specific condition.
Symptoms
Common Symptoms of Ulcerative Colitis
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) characterized by inflammation in the large intestine (colon and rectum). The most common symptoms of ulcerative colitis are abdominal pain and diarrhea, often with blood or pus. Patients may experience an urgency to defecate and may not be able to hold their bowel movements. The frequency of bowel movements can also increase, with some individuals having up to 20 or more episodes a day during severe flares.
Bowel Movement Changes
Changes in bowel habits are a hallmark of ulcerative colitis. Patients may notice a decrease in stool consistency, with stools often being loose or watery. The presence of blood in the stool is a significant symptom, resulting from the ulceration and inflammation of the intestinal lining. Additionally, individuals may experience rectal pain and a feeling of incomplete evacuation after a bowel movement.
Abdominal Pain and Cramping
Abdominal discomfort is a frequent symptom, which can range from mild to severe. The pain is often described as cramping and usually occurs before a bowel movement. The location of the pain can vary depending on which part of the colon is affected.
Weight Loss and Reduced Appetite
Weight loss is common in individuals with ulcerative colitis, often due to a reduced appetite. The chronic inflammation and abdominal pain can lead to decreased food intake. Additionally, frequent diarrhea and malabsorption can contribute to weight loss.
Fatigue and Anemia
Fatigue is a prevalent symptom, which may be due to the chronic nature of the disease, anemia, or as a side effect of the body's inflammatory response. Anemia in ulcerative colitis patients can result from chronic blood loss in the stool or from decreased iron absorption due to inflammation in the gut.
Fever
During a flare-up, some individuals may experience a low-grade fever as a result of the inflammation. A high fever is less common but can occur, especially if there is a severe infection or complication such as a perforation in the colon.
Dehydration and Electrolyte Imbalance
Chronic diarrhea can lead to dehydration and electrolyte imbalances. Symptoms of dehydration include thirst, dry mouth, decreased urine output, and lightheadedness. Electrolyte imbalances can cause symptoms such as muscle weakness, twitching, or irregular heartbeat.
Extraintestinal Symptoms
Ulcerative colitis can also cause symptoms outside of the digestive system, known as extraintestinal manifestations. These may include joint pain and swelling (arthritis), skin lesions, eye inflammation (uveitis), and liver disorders. These symptoms can occur even when the colitis itself is not active.
Growth Failure in Children
In pediatric cases, ulcerative colitis can affect growth and development. Children may experience delayed growth and puberty due to malnutrition, chronic inflammation, and the use of corticosteroids as part of their treatment regimen.
Severity of Symptoms
The severity of symptoms can vary widely among individuals with ulcerative colitis. Some may have mild symptoms, while others experience severe and debilitating symptoms that can significantly impact their quality of life. The course of the disease can also fluctuate, with periods of remission followed by relapses or flare-ups.
Complications
Complications of ulcerative colitis can include severe bleeding, a hole in the colon (perforation), severe dehydration, liver disease, and inflammation of the skin, joints, and eyes. In long-standing cases, there is an increased risk of colon cancer. Patients with ulcerative colitis may also experience a severe, acute complication known as toxic megacolon, where the colon rapidly expands and may become at risk of rupture.
Impact on Mental Health
Ulcerative colitis can also have an impact on mental health. The chronic nature of the disease, along with symptoms like pain, fatigue, and the social implications of frequent bowel movements, can lead to anxiety and depression in some individuals.
Summary of Symptoms
In summary, ulcerative colitis symptoms can range from mild to severe, affecting both the gastrointestinal tract and other parts of the body. The most common symptoms include abdominal pain, diarrhea with blood or pus, urgency to defecate, and weight loss. Extraintestinal manifestations and complications can also arise, affecting overall health and quality of life. It is important for individuals experiencing these symptoms to seek medical attention for proper diagnosis and management.
Cure
Current State of Cure for Ulcerative Colitis
As of the latest medical research and clinical practice, there is no definitive cure for ulcerative colitis (UC). Ulcerative colitis is a chronic condition that is characterized by periods of remission and exacerbation. While there is no cure, there are various treatment options available that aim to reduce symptoms, achieve and maintain remission, and improve the quality of life for those affected by the disease.
Medications Used in the Management of Ulcerative Colitis
The mainstay of treatment for ulcerative colitis involves the use of medications that modulate the immune system and reduce inflammation in the colon. These include aminosalicylates, corticosteroids, immunomodulators, and biologic agents. Aminosalicylates, such as mesalamine, are often used for mild to moderate cases and can be effective in maintaining remission. Corticosteroids are used for short-term control of acute flare-ups due to their potent anti-inflammatory effects, but they are not suitable for long-term use because of their side effects.
Immunomodulators, such as azathioprine and 6-mercaptopurine, can be used for those who do not respond to aminosalicylates or for maintenance of remission. Biologic agents, which include tumor necrosis factor (TNF) inhibitors like infliximab, adalimumab, and golimumab, as well as integrin receptor antagonists like vedolizumab, are used for moderate to severe ulcerative colitis, particularly when other treatments have failed.
More recently, small molecule drugs like tofacitinib, which is a Janus kinase inhibitor, have been approved for the treatment of moderate to severe ulcerative colitis. These medications offer new mechanisms of action and can be taken orally, providing another option for patients who have not responded to or cannot tolerate other treatments.
Surgical Options for Ulcerative Colitis
In cases where medical therapy does not control the symptoms, or if there are complications such as severe bleeding, perforation of the colon, or a high risk of cancer, surgery may be considered. The most common surgical procedure for ulcerative colitis is a proctocolectomy with ileal pouch-anal anastomosis (IPAA), which involves the removal of the colon and rectum and the creation of an internal pouch from the small intestine to restore bowel function.
While surgery is not a "cure" in the traditional sense, as it does not address the underlying cause of the disease, it does effectively eliminate the diseased tissue and can result in a significant improvement in quality of life. However, it is important to note that even after surgery, some patients may experience inflammation of the pouch, known as pouchitis, which can require ongoing management.
Off-Label Use of Medications in Ulcerative Colitis
Occasionally, medications approved for other conditions may be used off-label for ulcerative colitis when conventional therapies are ineffective. Off-label use is based on limited evidence or anecdotal experience, and such treatments are typically considered only after other options have been exhausted. Physicians may consider off-label use of medications in a carefully monitored setting, taking into account the potential risks and benefits for the individual patient.
Lifestyle and Dietary Considerations
While lifestyle and diet changes are not cures for ulcerative colitis, they can play a role in managing the disease. Patients are often advised to maintain a balanced diet and may find that certain foods exacerbate their symptoms. A dietitian can help in identifying trigger foods and in ensuring nutritional needs are met, especially during flare-ups when appetite and absorption may be affected.
Stress management techniques, such as meditation, exercise, and counseling, can also be beneficial as stress can sometimes trigger or worsen symptoms. Smoking cessation is particularly important, as smoking has been shown to exacerbate ulcerative colitis.
Future Directions in the Search for a Cure
Research into the pathogenesis of ulcerative colitis continues to advance, with the goal of developing a cure. Novel therapeutic targets are being explored, including new biologic agents and cell-based therapies such as stem cell transplantation. Clinical trials are ongoing for various potential treatments, and there is hope that these may one day lead to a cure or more effective management strategies.
It is also important to recognize the role of personalized medicine in the treatment of ulcerative colitis. As understanding of individual genetic and molecular profiles improves, it may be possible to tailor treatments more effectively to the individual patient, potentially improving outcomes and getting closer to a disease-free state.
Patients with ulcerative colitis should have regular consultations with their gastroenterologist to monitor their condition, assess response to therapy, and discuss any new research findings or treatments that may be applicable to their situation.
Access Ulcerative Colitis medicines today
If Ulcerative Colitis medicines are not approved or available in your country (e.g. due to supply issues), you can access them via Everyone.org.
How Everyone.org works

Make an enquiry
Choose the medicine you want to access, answer a couple of questions, and upload your prescription to speed things up. We’ll get back to you within 24 hours.


Make an enquiry
Choose the medicine you want to access, answer a couple of questions, and upload your prescription to speed things up. We’ll get back to you within 24 hours.


Breeze through the paperwork
We'll guide you through the required documents for importing unapproved medicine, ensuring you have all the necessary information.


Get a personalized quote
We’ll prepare a quote for you, including medicine costs and any shipping, administrative, or import fees that may apply.


Receive your medicine
Accept the quote and we’ll handle the rest - sourcing and safely delivering your medicine.

Some text on this page has been automatically generated. Speak to your physician before you start a new treatment or medication.
Let's talk
If you have any questions, call us or send us a message through WhatsApp or email:
Contact us